Park Bench
Take a seat on the bench and take a moment to consider the future.
Understanding holistic care
At the Park Bench, you will find information about your illness and how to manage your symptoms, as well as details on holistic support available.

The information provided is not a substitute for any advice given to you by your medical team. If you have any questions or any further concerns, talk to your medical team.
There are different sections to support you:
Why is it important to ensure a holistic approach to care?
|
|
A holistic approach looks at the needs of the whole person, not just your physical, mental or medical needs |
|
|
It is a team approach to address the needs of you and your loved ones, focusing on sensitive advanced care planning |
|
|
It may help to ensure that your preferences and decisions are respected |
By addressing physical, emotional and social needs, holistic care can help restore your sense of balance and enable you to take control of your illness, thereby improving your quality of life.1,2

Conversations about your goals and wishes can be useful at all stages of your disease journey.
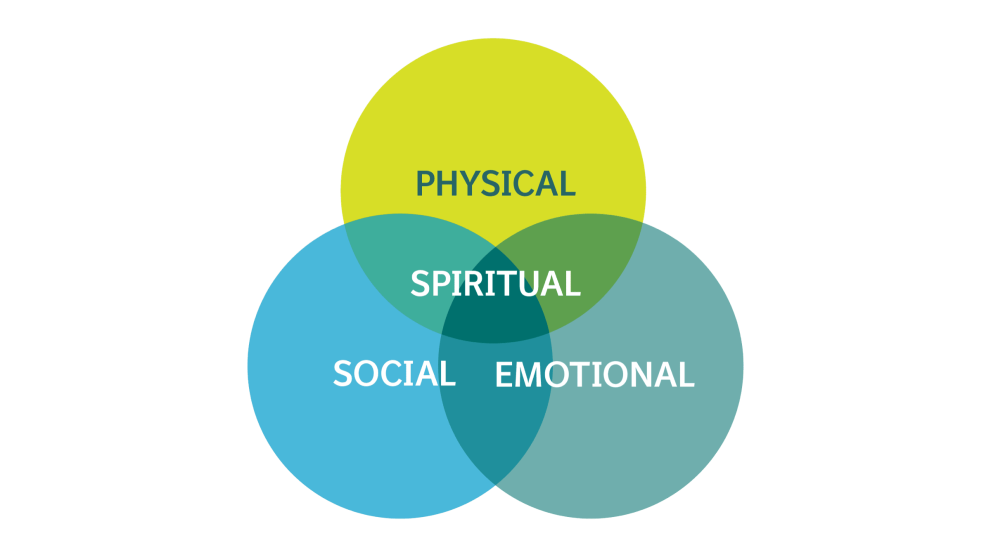
Holistic care brings together our physical health, how we feel, and how we interact with others, which are all interconnected but distinct facets of our well-being.
Looking to your future with holistic care
Holistic care planning
Engaging with holistic care
Holistic care aims to integrate psychological and spiritual aspects into patient care. This both affirms life and respects dying as a natural process.
Engaging with holistic care enables you to take control of your care and make informed decisions about the right path for you.

Talking to your healthcare team
This can be with your doctor or with a nurse; ask if your healthcare centre offers specialist holistic care support.
Talking to your family and loved ones
You don’t have to do this alone, your healthcare team and loved ones can support you through this.

Building confidence to discuss your needs and wishes
Planning holistic care can be difficult; by preparing yourself for difficult discussions, you can ensure the best outcomes for you.
Talking about your goals and wishes
Discussions about advanced care can be difficult. However, these challenging conversations will benefit you in the long run, as they ensure that everyone in your healthcare team, as well as your loved ones are aware of your wants and needs.
Some tips for starting a conversation about advanced care include:3
- Start by mentioning your worries, fears or wishes
- Seek clarification on any terminology that you are not sure about. Your medical team will be able to help!
- Choose a time and place when it is unlikely that you and other participants will be disturbed
- Remember that you don’t have to talk about everything at once! Different situations work for different people, and there’s no right or wrong way to start talking about the last stage of life
- Let the people you care about know how you feel about them
- Start with a question! This may help because it gives the other person a chance to say how they feel

Managing uncertainty
Planning ahead
Advanced care planning involves thinking and talking about your wishes for how you are cared for during the last stage of your life. Planning ahead can help you receive the care you want.
Planning ahead can help your loved ones, too. It is not an easy topic to think about, but, by discussing your wishes with your family and loved ones, you could be saving them from having to help doctors make difficult decisions later on without knowing what you would have wanted.
Where can I be cared for?
If you are approaching the last stage of life, you may be offered care in a variety of settings. Your healthcare team will organise for you to be cared for according to your wishes. You can receive holistic care:4
|
|
At home |
|
Holistic care can often be provided at home. Your GP can arrange for community nurses to come to your home and provide nursing care for you there |
|
|
|
In a care home |
|
You can receive holistic care in a care home, where trained staff are available to look after you day and night |
|
|
|
In a hospital |
|
You may be cared for in a hospital. Many hospitals have specialist holistic care teams who work alongside and support the healthcare team |
|
|
|
In a hospice |
|
Hospice care is provided by a specialist unit run by a team of doctors, nurses, social workers and counsellors |
Managing your illness
Managing the symptoms of your illness
A diagnosis of PPF brings up many thoughts, feelings and emotions. Some symptoms of PPF, such as breathlessness and fatigue, can also impact your mood.
It is common for people with PPF to experience depression, anxiety or stress.5 Fortunately, there are things you can do to help you feel better.

Managing breathlessness

Managing mental health and well-being
Managing fatigue
Dealing with persistent fatigue can have a significant effect on a person’s quality of life.
Fatigue in patients with PPF may occur due to a combination of factors such as decreased oxygen levels, sleep difficulties and emotional distress.
- Consider light exercise routines to develop exercise capacity and improve energy levels
- Consider breaking activities into smaller tasks and pacing yourself throughout the day
- Take a break when you need it and learn how to say “no”
- Practice good sleep habits to improve sleep quality and reduce fatigue
- Talk to your doctor about any symptoms you are experiencing
Making decisions about your healthcare
What to consider when speaking with your healthcare team
There is no set way to plan ahead, but there are some useful steps that may help you. If you are unsure or wish for further advice, consult your GP, community nurse or another member of your healthcare team.
Take a moment to reflect on what matters most to you and begin developing your holistic care plan. Think about and take note of:
Your needs and wishes for a care plan
Making the most of your treatments, for example:
- A breathing technique that helps me is:
- A healthy food to eat when I feel nauseous is:
- When I feel anxious I:
Your goals and how to achieve them, for example:
- What is my goal?
- What will I do to achieve this?
- When I feel anxious I:
- Who could help me?
Taking notes
Additional information

Picnic Area
References
- Jasemi M, et al. Indian J Palliat Care 2017;23:71–80;
- The National Council for Palliative Care. Every Moment Counts. Available at: https://www.nationalvoices.org.uk/sites/default/files/public/publications/every_moment_counts.pdf. Last accessed: February 2023;
- NHS. Starting to talk about your illness/End of life care. Available at: https://www.nhs.uk/conditions/end-of-life-care/starting-to-talk-about-your-illness/. Last accessed: February 2023;
- NHS. Where you can be cared for/End of life care. Available at: https://www.nhs.uk/conditions/end-of-life-care/where-you-can-receive-care/. Last accessed: February 2023;
- Pulmonary Fibrosis M.D. Depression and Pulmonary Fibrosis. Available at: https://pulmonaryfibrosismd.com/depression-and-pulmonary-fibrosis/. Last accessed: February 2023;
- Pulmonary Fibrosis M.D. Combating fatigue in Pulmonary Fibrosis. Available at: https://pulmonaryfibrosismd.com/combating-fatigue-pulmonary-fibrosis/. Last accessed: February 2023.
NP-GB-103033 | July 2024
|
If you live in the UK and you experience any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in the package leaflet. You can also report side effects directly via the yellow card scheme at https://yellowcard.mhra.gov.uk/. By reporting side effects, you can help provide more information on the safety of this medicine. If you live in the Republic of Ireland and you experience any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in the package leaflet. You can also report side effects directly via the Health Products Regulatory Authority at www.hpra.ie or by email to medsafety@hpra.ie. By reporting side effects, you can help provide more information on the safety of this medicine. |
THIS WEBSITE HAS BEEN DEVELOPED BY BOEHRINGER INGELHEIM AND IS INTENDED FOR PEOPLE WITH PROGRESSIVE PULMONARY FIBROSIS WHO HAVE BEEN PRESCRIBED OFEV® (NINTEDANIB).
This website is intended for people with progressive pulmonary fibrosis who have been prescribed treatment with OFEV® (nintedanib). OFEV® is used to treat idiopathic pulmonary fibrosis (IPF), or other chronic fibrosing interstitial lung diseases (ILDs) that are showing signs of progression and these diseases are referred to on this website collectively as ‘progressive pulmonary fibrosis’ (PPF).
This website aims to provide you with information about your disease and how to manage your symptoms or the side effects of your treatment, as well as to give you details on holistic support available.
The information on this website has been developed to enhance, but not replace, the advice and help of your medical team. If you have any questions after reading this website, or any further concerns, always talk to your medical team – i.e., a nurse, doctor or pharmacist – they are here to help you.
You’ll also find more information about OFEV® in your Patient Information Leaflet (PIL), included with your OFEV® medication pack, or on https://www.medicines.org.uk/emc/files/pil.7705.pdf if you live in Great Britain, or on https://www.emcmedicines.com/en-gb/northernireland/medicine?id=1c9c7bb7-cac4-4c5f-a633-a8220c0a16dd&type=pil if you live in Northern Ireland or on https://www.medicines.ie/medicines/ofev-150-mg-soft-capsules-33198/patient-info if you live in the Republic of Ireland.